An ectopic pregnancy is not only a medical condition, but it is often a deeply impactful experience that leaves both physical and emotional scars. This is especially true for women who have undergone treatment involving fallopian tube removal (salpingectomy), whether on the left or right side.
After treatment, many couples share the same concerns:
After fallopian tube removal, is there still a risk of another ectopic pregnancy?
How much does the chance of a natural pregnancy decrease?
If planning for another pregnancy, how can it be done safely while reducing the risk of recurrence?
To help couples better understand their situation and prepare with confidence, this article explains the condition in a structured, evidence-based way—so prospective parents can better understand their bodies and plan their next pregnancy safely.
Does an Ectopic Pregnancy Always Require Fallopian Tube Removal?
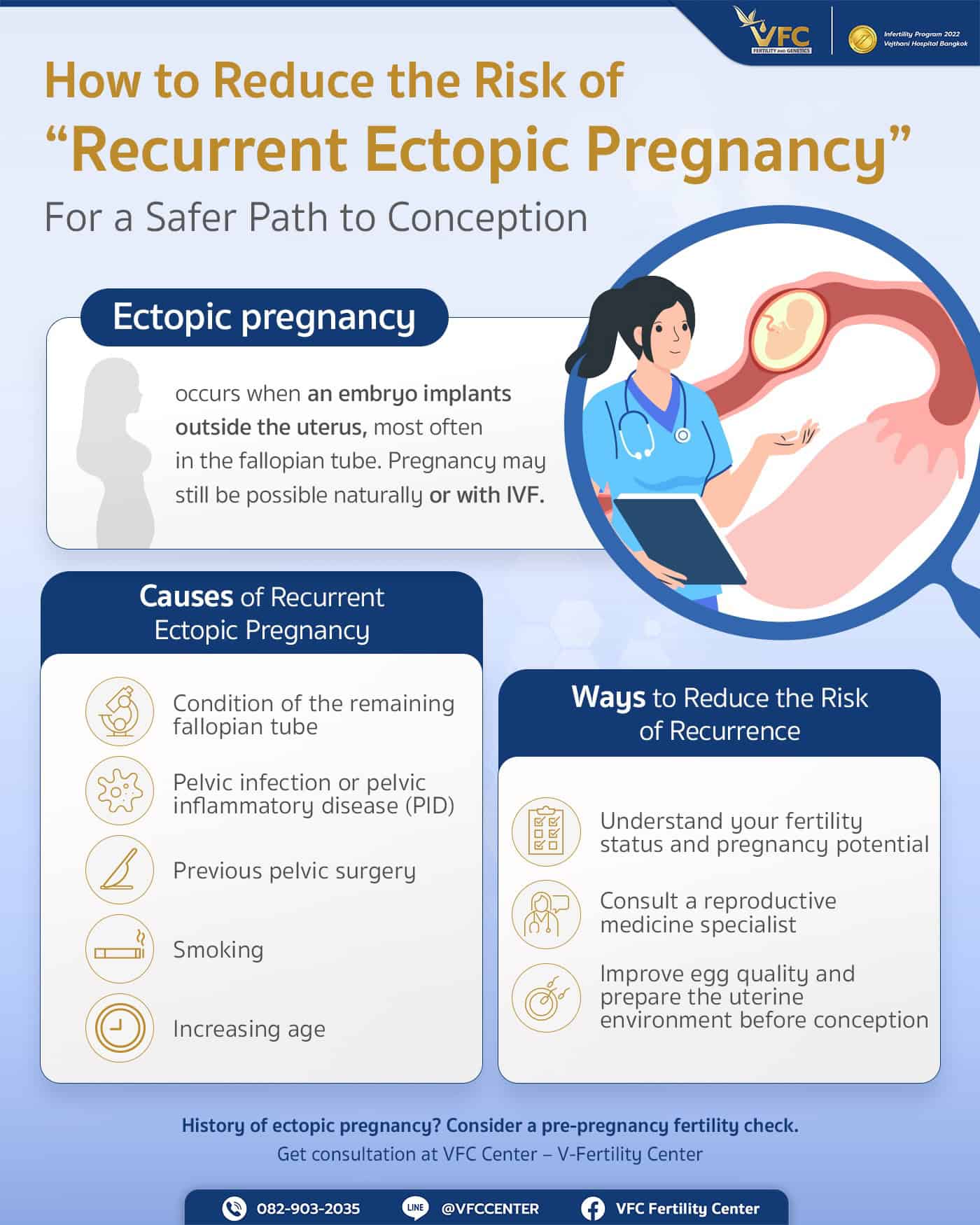
An ectopic pregnancy is a condition in which the embryo implants outside the uterine cavity, most commonly within the fallopian tube. If the embryo continues to grow, the narrow fallopian tube may rupture, leading to internal bleeding. This is a life-threatening medical emergency that requires immediate treatment.
Not all cases of ectopic pregnancy require removal of the fallopian tube. Treatment decisions depend on several factors, including:
- Size of the ectopic mass
- hCG hormone levels
- Condition of the fallopian tube (ruptured, near rupture, or intact)
- Blood pressure and overall hemodynamic stability of the patient
In mild cases, medication or tube-preserving surgery may be possible. However, if the tube has ruptured, bleeding is severe, or the tube is already significantly damaged, surgical removal of the affected fallopian tube is often necessary to control bleeding and prevent serious complications. This approach also helps reduce the risk of recurrent ectopic pregnancy in the same tube.
Can You Still Get Pregnant After Fallopian Tube Removal?
Yes. Most women can still become pregnant after a salpingectomy if the remaining fallopian tube is healthy. According to data from the Miscarriage Association in the UK, approximately 65% of women conceive again within 18 months after treatment, increasing to around 85% within two years—even after losing one fallopian tube.
This is because both ovaries continue to function normally, and the remaining fallopian tube can sometimes capture an egg released from either ovary. Losing one tube does not mean pregnancy is impossible, but success depends on the health of the remaining tube and other fertility factors.
Consult a reproductive medicine specialist to plan pregnancy after an ectopic pregnancy.
Risk of Recurrent Ectopic Pregnancy After Salpingectomy
Even after the affected fallopian tube is removed, recurrence is still possible. The embryo must still travel through the remaining tube before reaching the uterus. The risk of recurrent ectopic pregnancy is estimated at 7-10%, or about 1 in 10 cases.
For patients who preserved the previously affected tube, the risk may be slightly higher.
Causes of Ectopic Pregnancy Recurrence Couples Should Know
- Health of the remaining fallopian tube: Scarring, narrowing, or chronic inflammation can obstruct embryo transport, increasing implantation risk outside the uterus.
- History of pelvic inflammatory disease (PID): Often caused by sexually transmitted infections, PID can damage both tubes.
- Previous pelvic surgery: Surgeries such as ovarian cyst removal or uterine surgery may increase adhesions.
- Smoking: Nicotine and toxins impair ciliary function inside the fallopian tubes, disrupting egg and embryo movement.
- Advanced maternal age: Egg quality and tubal function may decline, increasing abnormal embryo transport.
Pregnancy is still possible despite tubal issues with assisted reproductive technology at VFC Center
Post-Treatment Follow-Up to Reduce the Risk of Recurrent Ectopic Pregnancy
After treatment, future planning should focus on uterine health, fallopian tube condition, and safe pregnancy planning. Four key areas should be addressed:
Fallopian Tube and Uterine Evaluation Before Pregnancy
Recommended assessments include:
- Transvaginal ultrasound to evaluate the uterus, ovaries, and adhesions
- Hysterosalpingography (HSG) to assess tubal patency
- Laparoscopy in selected cases when adhesions or other gynecologic conditions are suspected
These evaluations help determine whether natural conception is advisable or if assisted reproductive technology should be considered.
Lifestyle Adjustments to Reduce Inflammation and Risk Factors
- Stop smoking and avoid secondhand smoke
- Prevent and treat pelvic infections; use condoms if at risk
- Get adequate rest, manage stress, and maintain overall health
Considering IVF After a Previous Ectopic Pregnancy
If the remaining fallopian tube is severely damaged or risk factors are high, physicians may recommend IVF. This approach fertilizes the egg outside the body and transfers the embryo directly into the uterus, greatly reducing reliance on the fallopian tubes.
Close Monitoring During Early Pregnancy
Whether conceiving naturally or via ICSI, women with a prior ectopic pregnancy should undergo:
- Serial hCG blood tests to assess hormone trends
- Transvaginal ultrasound at 5-6 weeks to confirm intrauterine pregnancy
Early monitoring allows prompt detection and prevention of serious complications.

Practical Guidance for Pregnancy After Ectopic Pregnancy and Salpingectomy
Preparing the body properly is a key factor in effectively reducing the risk of recurrent ectopic pregnancy and improving the chances of a successful pregnancy as planned. The following are recommended guidelines for couples to follow.
Understand Your Personal Fertility Outlook
While many women can conceive naturally, success depends on age, egg quality, sperm quality, hormonal balance, and conditions such as endometriosis or PCOS.
Consult a Reproductive Medicine Specialist
Specialists can assess remaining tubal health, evaluate fertility factors in both partners, and advise whether natural conception or ICSI is the safest approach.
Improve Egg Quality and Prepare the Uterine Environment
- Maintain a healthy weight
- Eat a balanced diet; supplement folic acid as advised
- Avoid smoking and alcohol
- Exercise moderately
If you have a history of ectopic pregnancy, a comprehensive fertility evaluation is a critical first step. At VFC Center (V Fertility Center), we provide personalized fertility assessments by reproductive medicine specialists—helping couples plan a safe and successful pregnancy journey, including a complete infertility check in Bangkok.
Article by Dr. Worawat Siripoon
Contact or Book a Consultation:
VFC Center – V-Fertility Center
Hotline: 082-903-2035
LINE Official: @vfccenter
Frequently Asked Questions (FAQs)
Q : What symptoms may indicate a recurrent ectopic pregnancy?
A : Lower abdominal pain (often one-sided), vaginal bleeding, dizziness, shoulder pain, or fainting should prompt immediate medical attention.
Q : Do pelvic adhesions increase the risk of recurrence?
A : Yes. Adhesions can distort tubal anatomy and trap the embryo before it reaches the uterus.
Q : What is the most effective way to reduce recurrence risk?
A : Comprehensive fertility evaluation and, in some cases, choosing IVF to bypass the fallopian tubes.
Q : Does the male partner play a role in ectopic pregnancy risk?
A : Not directly, but sexually transmitted infections or poor sperm quality may indirectly contribute to reproductive complications.

OBSTETRICS AND GYNAECOLOGY-REPRODUCTIVE MEDICINE





No Comments
Sorry, the comment form is closed at this time.