
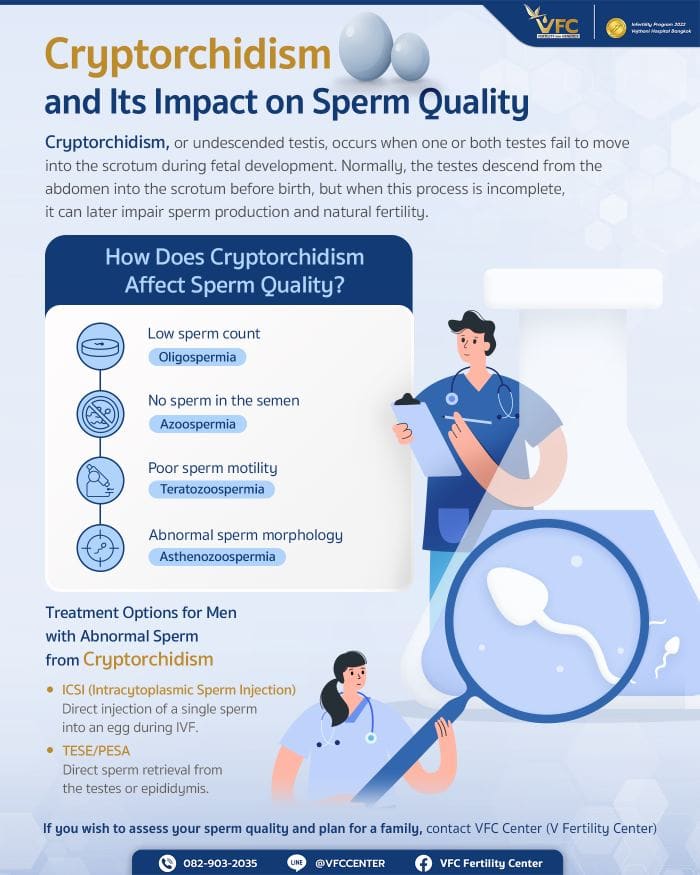
Cryptorchidism is a condition where one or both testicles fail to descend into the scrotum before birth. This can negatively impact sperm quality and lead to male infertility, especially if left untreated. While surgery during infancy can help preserve fertility, many men with a history of cryptorchidism still experience low sperm count, poor motility, or no sperm in the ejaculate. Fortunately, modern fertility treatments like ICSI and TESE sperm retrieval offer effective solutions for conception.
For many couples planning to start a family, understanding the factors that influence fertility is crucial. One of the most important aspects on the male side is sperm quality. Among congenital abnormalities that can significantly affect it is cryptorchidism, commonly referred to in Thai as “undescended testis” or “ภาวะทองแดง.”
This article explores cryptorchidism in depth—from its causes and physiological mechanisms to its impact on sperm production and the available medical and reproductive-technology treatments.
What Is Cryptorchidism?
Cryptorchidism, or undescended testis, is a congenital condition in males in which one or both testes fail to descend into the scrotum during fetal development.
Normally, a male fetus’s testes form in the abdomen near the kidneys early in gestation and gradually descend through the inguinal canal into the scrotum during the last 2–3 months before birth. This process is regulated by complex hormonal (particularly testosterone) and anatomical factors. Because of this timing, cryptorchidism occurs more frequently in premature infants, whose testes have not yet completed the descent.
The undescended testis may be unilateral or bilateral, and it can arrest at various points along the descent pathway—within the abdomen (intra-abdominal), in the groin (inguinal), or above the scrotum (suprascrotal).
It is important to differentiate cryptorchidism from a retractile testis, in which the testis is already in the scrotum but can be pulled temporarily upward by a strong cremasteric reflex when the child is cold or startled. Retractile testes usually descend normally with growth and rarely require surgery.
Why Does Testicular Position Matter?
One might wonder why nature places the testes—the body’s “sperm factories”—outside the body cavity rather than keeping them inside like other organs.
The answer lies in temperature regulation.
Testicular function requires a temperature about 2–3 °C lower than core body temperature to support normal spermatogenesis. If a testis remains in the abdomen or groin, the higher heat environment causes testicular heat stress, which directly disrupts sperm production and can lead to premature degeneration of testicular tissue.
In addition, mispositioned testes are at increased risk of testicular torsion and testicular cancer, which is why early diagnosis and treatment of cryptorchidism are strongly recommended in childhood.
How Does Cryptorchidism Affect Sperm Quality?
The damage from the aforementioned high temperatures is the primary link between cryptorchidism and male infertility. It can impact sperm quality in several ways:
1. Low Sperm Count (Oligospermia)
Heat damages the sperm-producing germ cells, causing the “factory” to produce significantly fewer sperm. This results in a total sperm count below the standard threshold (less than 15 million sperm per milliliter).
2. No Sperm in Ejaculate (Azoospermia)
In severe cases, especially in patients with bilateral cryptorchidism that was not treated or was treated too late, the heat may completely destroy the germ cells. This stops sperm production entirely, resulting in no sperm being found in the semen.
3. Abnormal Sperm Motility (Asthenozoospermia)
High temperatures not only affect “production” but also disrupt the “maturation” process, which occurs in the epididymis (the tube attached to the testis). This leads to poor sperm quality, where sperm swim poorly or not at all (low percentage of progressive motility), creating a major obstacle to reaching and fertilizing an egg.
4. Abnormal Sperm Morphology (Teratozoospermia)
Spermatogenesis is an extremely delicate process. Abnormal heat interferes with sperm formation, leading to a high number of abnormally shaped sperm (e.g., round heads, pinheads, no tail, or double tails). These abnormally shaped sperm are typically unable to penetrate the egg’s outer layer to achieve fertilization.
Want to know your sperm quality ? Visit VFC Center for a semen analysis.
Diagnosis and Treatment
Cryptorchidism is often detected at birth during a pediatric physical exam. If one or both testes are not in the scrotum, the physician may initially recommend observation for the first 3–6 months, as some testes may descend spontaneously.
If descent does not occur, the standard treatment is orchiopexy—a surgical procedure to move and fix the testis into the scrotum—ideally performed between 6 and 12 months of age. Early correction allows normal testicular development and significantly lowers the future risk of infertility.
In cases where the testis cannot be felt, imaging such as ultrasound or laparoscopy may be required to locate it.
If You Had Cryptorchidism in Childhood—Can It Still Affect Fertility Now?
Yes, it can. Even after successful surgery in childhood, there remains an increased likelihood of reduced sperm quality, for two main reasons:
- Pre-existing Damage:
The time the testis remained in the warmer abdominal cavity—sometimes as little as six months—may have caused irreversible loss of germ cells before surgery. - Intrinsic Abnormality:
In many patients, the failure of descent itself may indicate underlying developmental or hormonal defects in the testis, meaning function may remain suboptimal even after proper positioning.
The risk of infertility is higher in men with bilateral cryptorchidism than those with a unilateral condition, since the normal testis in unilateral cases can often compensate.
Men with a history of cryptorchidism who plan to conceive should therefore consult a reproductive specialist and undergo semen analysis to evaluate their current fertility potential.

Treatment Options for Abnormal Sperm from Cryptorchidism
If your semen analysis reveals suboptimal sperm quality—whether it’s low count, poor motility, abnormal shape, or even no sperm at all (Azoospermia)—it does not mean you cannot become a father. Modern assisted reproductive technology (ART) is advanced enough to overcome many of these obstacles.
1. ICSI (Intracytoplasmic Sperm Injection)
For patients with a low sperm count, poor motility, or poor morphology, ICSI is the most effective solution. This process involves selecting the single best-looking sperm (even if very few are available) and injecting it directly into the egg to assist fertilization. It bypasses the need for millions of sperm or their ability to swim.
2. TESE/PESA (Sperm Retrieval Directly from the Testis)
For patients with Azoospermia (no sperm in the ejaculate) due to a history of cryptorchidism, there is still hope. In many cases, the testes may still be producing very small amounts of sperm that are simply not present in the ejaculate. A doctor can retrieve sperm directly using:
- PESA (Percutaneous Epididymal Sperm Aspiration): Using a fine needle to aspirate sperm from the epididymis (the maturation tube).
- TESE (Testicular Sperm Extraction): This is a form of TESE sperm retrieval where a minor surgical procedure is performed to remove small samples of testicular tissue. A high-powered microscope may then be used (Microdissection TESE) to find sperm hidden within that tissue.
Even a few retrieved sperm can be used immediately for ICSI.
For men with a history of cryptorchidism who are planning a family, assessing sperm quality is a vital, non-negotiable step to clearly and accurately understand your reproductive potential. At VFC Center (V Fertility Center), we elevate Semen Analysis with our CASA (Computer-Assisted Semen Analysis) program. This advanced technology uses a high-resolution computer system to analyze sperm count, morphology (shape), and motility patterns with high efficiency. In cases where sperm are not present in the semen, procedures such as TESE sperm retrieval can be considered alongside these detailed assessments. This precise data allows our team of reproductive specialists to design the most appropriate and targeted treatment plan for you, turning past health concerns into confidence on your path to parenthood.
Frequently Asked Questions (FAQs)
Q: If only one testis was undescended, can I still father a child naturally?
A: The chances are generally good, though some men may still experience below-average semen parameters. Even if the normal testis compensates hormonally and functionally, overall sperm quality may remain reduced. A semen analysis is the best first step for accurate assessment.
Q: Does the age at surgery—1 year vs 10 years—make a difference for fertility?
A: Yes, dramatically. The longer the testis remains exposed to body heat, the greater the permanent loss of germ cells. Surgery performed between 6 and 12 months offers the best chance to preserve fertility potential, whereas correction at age 10 is often too late to prevent damage.
Q: Does cryptorchidism increase the risk of testicular cancer, and does surgery eliminate that risk?
A: Men with a history of cryptorchidism are indeed several times more likely to develop testicular cancer. Orchiopexy does not eliminate the risk but allows easier self-examination and early detection because the testis is now accessible within the scrotum.
Q: I had surgery for cryptorchidism as a child and now plan to have children. What should I do first?
A: Don’t wait years trying naturally. If you have a history of undescended testis, consult a fertility specialist and undergo semen analysis immediately. The results will show whether your sperm quality has been affected and guide the next steps for timely treatment.
Article by Dr. Worawat Siripoon
Contact or Book a Consultation:
VFC Center – V-Fertility Center
Hotline: 082-903-2035
LINE Official: @vfccenter

OBSTETRICS AND GYNAECOLOGY-REPRODUCTIVE MEDICINE





No Comments
Sorry, the comment form is closed at this time.