
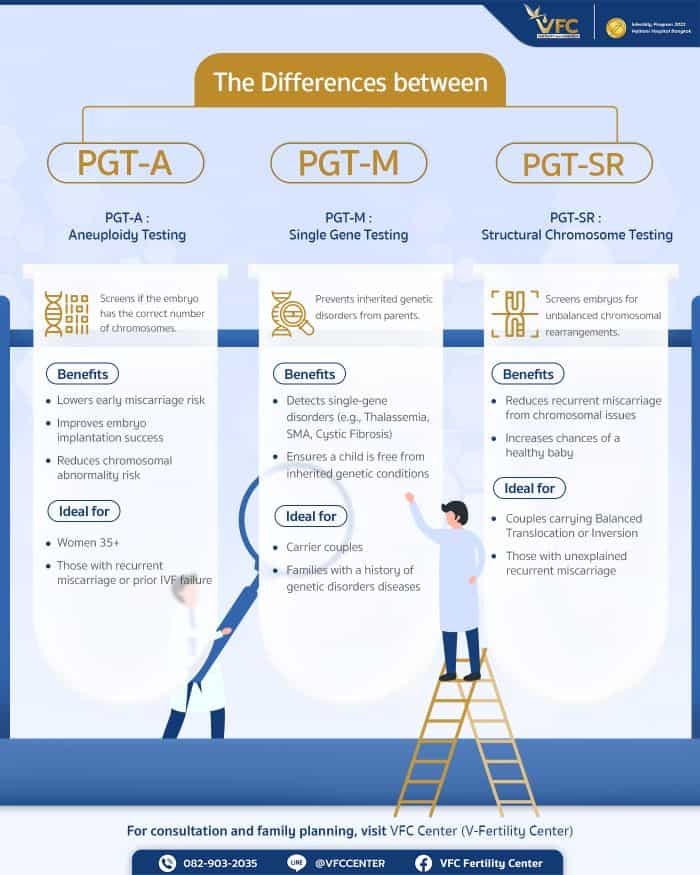
PGT-A, PGT-M, and PGT-SR are advanced preimplantation genetic testing methods that help improve IVF/ICSI success by selecting embryos with the lowest risk of chromosomal or genetic abnormalities. While PGT-A focuses on chromosome number, PGT-M targets specific inherited diseases, and PGT-SR screens for structural chromosomal rearrangements. Choosing the right test based on medical history, age, and genetic risk allows couples to reduce miscarriage risk, improve implantation rates, and increase the chance of a healthy pregnancy, especially when undergoing PGT-A testing in Thailand at a specialised fertility centre.
Assisted reproductive technologies in 2025 are moving toward highly personalized fertility care, driven by more precise preimplantation genetic testing (PGT).
This article walks couples planning for parenthood through the differences between PGT-A, PGT-M, and PGT-SR. Highlighting how each test works, which conditions they are designed for, and how they can help maximize pregnancy success throughout the IVF/ICSI journey.
What Is PGT and Why Is It Important in Fertility Treatment?
PGT (Preimplantation Genetic Testing) is a technique used to analyze the genetic makeup of embryos before they are transferred into the uterus during IVF/ICSI. The goal is to analyze embryos to identify those that:
- Have a normal number of chromosomes (related to PGT-A)
- Are free from hereditary single-gene disorders (related to PGT-M)
- Have a normal or balanced chromosomal structure (related to PGT-SR)
By examining chromosomal or genetic abnormalities before transfer, physicians can select embryos with the lowest risk of miscarriage, implantation failure, or congenital disorders. This is especially important for women over age 35, couples with a history of unexplained recurrent miscarriage, or couples with a family history of genetic disorder.
Benefits of PGT: Reducing Miscarriage and Genetic Risks
PGT helps fertility specialists identify embryos with minimal risk of chromosomal or genetic abnormalities. Key benefits include:
- Increased chances of successful pregnancy, particularly for women of advanced maternal age or couples with recurrent pregnancy loss
- Reduced risk of first-trimester miscarriage caused by chromosomal abnormalities
- Lower likelihood of congenital disorders, such as Down syndrome and other genetic diseases
- Reduced the need to transfer multiple embryos, minimizing the risk of twin or multiple pregnancies
Factors Physicians Consider Before Selecting a PGT Method
Choosing the most appropriate type of PGT requires careful consideration of several medical factors and the couple’s history, such as:
- Maternal age: Especially for women aged 35 and older, as the risk of embryos having chromosomal abnormalities (aneuploidy) increases significantly.
- Family medical history: If there is a known hereditary genetic disorder in the family, such as thalassemia or spinal muscular atrophy, physicians may recommend genetic testing to detect potential gene mutations.
- History of miscarriage: Couples with two or more miscarriages, particularly in the first trimester, are often advised to undergo PGT, since chromosomal abnormalities in embryos are a common cause.
- Previous IVF/ICSI failures: Even after transferring high-quality embryos, some couples experience implantation failure. In such cases, additional genetic screening is recommended before starting a new IVF/ICSI cycle.
Consultation for PGT-A, PGT-M, and PGT-SR is available at VFC Center
Types of PGT for Embryo Genetic Screening
Preimplantation genetic testing (PGT) is divided into three main categories, each designed to detect different genetic or chromosomal issues. While they share the common goal of improving pregnancy success and reducing miscarriage risk, each test serves a distinct purpose depending on the couple’s medical needs.
PGT-A Chromosomal Screening for Embryo Aneuploidy
PGT-A (Preimplantation Genetic Testing for Aneuploidy) examines whether an embryo has the correct number of chromosomes, 46 in total, or whether there are missing chromosomes (monosomy) or extra chromosomes (trisomy). These abnormalities commonly cause Down syndrome (Trisomy 21), miscarriage, or failure of the embryo to implant or develop normally.
Benefits of PGT-A
- Helps identify embryos with a normal number of chromosomes (euploid embryos)
- Reduces the likelihood of early miscarriage
- Improves embryo implantation rates and overall pregnancy success
- Minimizes risks related to embryo aneuploidy that may affect fetal health
Who Is a Good Candidate for PGT-A?
- Women aged 35 and older
- Couples with unexplained recurrent miscarriage
- Couples who have experienced multiple failed IVF/ICSI cycles
- Individuals seeking to reduce the risk of chromosomal abnormalities in their baby
PGT-M Gene-Level Screening for Specific Genetic Disorders
PGT-M (Preimplantation Genetic Testing for Monogenic/Single Gene Disorders) detects known mutations in single genes responsible for inherited diseases passed down from one or both parents. Examples include thalassemia, cystic fibrosis, and spinal muscular atrophy (SMA).
Benefits of PGT-M
- Prevents severe hereditary diseases from being passed to the next generation
- Reduces the risk of conceiving a child with a serious genetic disorder
- Offers peace of mind for families with known genetic conditions
Who Is a Good Candidate for PGT-M?
- Couples who are carriers of serious single-gene disorders
- Couples who previously had a child diagnosed with a genetic disease
- Individuals with a strong family history of hereditary genetic conditions
PGT-SR Screening for Structural Chromosomal Rearrangements
PGT-SR (Preimplantation Genetic Testing for Structural Rearrangements) is designed for couples in which one partner carries a structural chromosomal rearrangement, such as a balanced translocation or inversion. Although carriers are usually healthy, they have an increased risk of producing embryos with unbalanced chromosomal structure, leading to recurrent miscarriage, failed pregnancies, or severe congenital disorders.
A balanced translocation occurs when two chromosomes exchange segments without losing or gaining genetic material. Problems arise during the formation of eggs or sperm, increasing the chance of embryos with missing or extra chromosomal segments.
Benefits of PGT-SR
- Helps distinguish embryos with structural abnormalities from those with normal or balanced chromosomes
- Reduces the risk of recurrent miscarriage caused by chromosomal rearrangements
- Enables the selection of embryos that are euploid or balanced, improving pregnancy success
- Provides reassurance for couples with a history of chromosomal issues
- Increases the chance of having a healthy baby without structural chromosome abnormalities
Who Is a Good Candidate for PGT-SR?
- Couples with two or more unexplained miscarriages
- Couples known to carry a balanced translocation or inversion
- Individuals who previously had a fetus or child with structural chromosomal abnormalities
- Couples who want to minimize the risk of passing structural chromosomal issues to future generations
Summary of Key Differences Between PGT-A, PGT-M, PGT-SR
- PGT-A screens for abnormalities in chromosome number (aneuploidy), such as missing or extra chromosomes.
-
- PGT-M examines single-gene mutations, such as thalassemia, SMA, or cystic fibrosis. Ideal for couples who are carriers of hereditary gene disorders.
- PGT-SR analyzes chromosomal structure, helping identify embryos affected by parental chromosomal rearrangements such as translocation or inversion. This method reduces miscarriage risk and increases the chance of a healthy pregnancy.
Schedule a consultation for PGT-A, PGT-M, or PGT-SR at VFC Center
Recommendations for Chromosomal and Genetic Embryo Screening

- Consult with a reproductive specialist to determine whether PGT-A, PGT-M, or PGT-SR is appropriate for your case
- Prepare your body for egg and sperm collection with adequate rest, a nutritious diet, and stress reduction
- Understand that PGT is a screening tool, not a genetic modification technique
- Be aware of test limitations and review results closely with your physician
- Coordinate treatment and embryo transfer planning with a multidisciplinary fertility team
Preimplantation genetic testing (PGT-A, PGT-M, PGT-SR) empowers individuals facing infertility to select healthy embryos, reduce miscarriage risk, and enhance confidence in their IVF/ICSI success.
For fertility consultation or genetic screening guidance, including PGT-A testing in Thailand, visit VFC Center, a leading fertility technology hub offering comprehensive reproductive care, from genetic analysis to personalized treatment planning. Our specialists are committed to helping every family welcome a healthy baby.
Frequently Asked Questions (FAQs):
Q: Is PGT painful, and how long does the process take?
A: PGT itself is not painful because the biopsy step is performed on embryos in the laboratory following IVF or ICSI. It does not affect your body or harm the embryo. Testing usually takes 1–2 weeks, depending on the type of PGT (PGT-A, PGT-M, or PGT-SR) and the laboratory process used.
Q: Does PGT really increase the chances of a successful pregnancy?
A: Yes. Extensive medical data show that PGT-A, PGT-M, and PGT-SR significantly improve pregnancy success rates by helping identify embryos that are chromosomally normal and healthy (euploid). This reduces miscarriage, failed implantation, and risks of genetic disorders—especially for women over 35 or couples with a history of recurrent pregnancy loss.
Q: Are there limitations or risks associated with PGT?
A: While PGT is highly effective at reducing the risk of transferring abnormal embryos, it has limitations. It cannot guarantee pregnancy because factors such as uterine health and overall well-being also play a role. Some very small chromosomal abnormalities (microdeletions or microduplications) may not be detectable. Additionally, PGT must be performed as part of an IVF/ICSI cycle.
For these reasons, it is recommended to consult a reproductive specialist to determine suitability and create a personalized treatment plan.
Article by: Dr. Wanakan Singhasena
Contact or Book a Consultation:
VFC Center – V-Fertility Center
Hotline: 082-903-2035
LINE Official: @vfccenter

OBSTETRICS AND GYNAECOLOGY-REPRODUCTIVE MEDICINE





No Comments
Sorry, the comment form is closed at this time.