Preparation for pregnancy begins with proper health care and screening, particularly female hormone testing. This test is crucial for evaluating reproductive system readiness and increasing the chances of conception.
In this article, we explain the importance of female hormone testing and provide guidance on how to prepare effectively before trying to conceive.
What is Female Hormone Testing and Why Is It Important?
Female hormone testing measures hormone levels in the body to assess the functionality of the reproductive system, especially FSH and AMH. These markers help evaluate whether the ovaries and egg production processes are functioning properly.
FSH and AMH are key indicators for assessing pregnancy readiness. Testing these hormones before conception allows couples to understand their body’s status and better prepare for a healthy pregnancy.
What is FSH (Follicle-Stimulating Hormone)?
FSH (Follicle-Stimulating Hormone) is secreted by the anterior pituitary gland and plays a vital role in stimulating the growth of follicles in the ovaries, which is essential for ovulation during each menstrual cycle.
FSH levels fluctuate according to the menstrual cycle. They rise during the early cycle (around days 2–5) to stimulate egg growth and decrease once enough estrogen is produced by the mature follicle.
Understanding FSH Levels
1. High FSH Levels :
May indicate declining ovarian function, perimenopause, or premature ovarian insufficiency (POI). The body secretes more FSH to stimulate the ovaries, but if ovarian response is low, FSH rises abnormally as a compensatory mechanism.
- Examples of conditions with high FSH
- Ovarian failure
- Premature menopause (POI)
- Women over 35 experiencing reduced egg count
2. Low FSH Levels :
Could reflect pituitary hormone secretion issues or disruptions in the hormonal system, such as low sex hormones or irregular ovulation.
- Examples of conditions with low FSH
- Polycystic Ovary Syndrome (PCOS)
- Hormonal imbalance from the hypothalamus or pituitary gland
- Chronic stress, underweight, or excessive exercise
Optimal FSH Levels for Pregnancy
- Low to moderate FSH (5–10 IU/L): Normal for women of reproductive age and indicates the ovaries are likely responsive.
- FSH 10–15 IU/L: Caution, may indicate diminished ovarian reserve or fewer eggs.
- FSH >20 IU/L: Especially in older women, this indicates reduced natural fertility and may require fertility treatments.

What is AMH (Anti-Müllerian Hormone)?
AMH is produced by granulosa cells surrounding eggs in ovarian follicles. While it does not directly regulate the menstrual cycle, it is essential for evaluating ovarian reserve—the number of remaining eggs—which is critical for women planning pregnancy.
AMH testing is widely used to assess how long the ovaries can produce eggs. It does not depend on the menstrual cycle and can be performed on any day.
What Do AMH Levels Indicate?
1. High AMH
Indicates a high number of eggs, often found in early reproductive age or women with multiple ovarian cysts (PCOS). High levels may suggest good ovarian response but can also indicate hormonal imbalance or irregular ovulation.
2. Low AMH
Reflects decreased egg quantity due to aging, genetics, ovarian surgery, chemotherapy, or other factors causing premature ovarian decline. Low AMH may signal higher infertility risk, warranting early intervention or egg preservation.
AMH Reference Levels
| AMH Level (ng/mL) |
General Meaning |
| >3.0 | Very good ovarian response (may be associated with PCOS) |
| 1.5-3.0 | Normal, suitable for pregnancy |
| 1.0-1.5 | Moderate, showing early decline in eggs |
| <1.0 | Low, indicating reduced ovarian reserve |
| <0.5 | Risk of ovarian insufficiency, early treatment recommended |
Preparing for Pregnancy Through Hormone Testing
Why Test Female Hormones 3–6 Months Before Conception?
- Allows time to balance hormones: If abnormal levels are detected, doctors may suggest lifestyle adjustments or hormone therapy, which requires time to take effect.
- Facilitates treatment planning: For instance, extremely low AMH may require egg freezing or fertility treatments.
- Prepares the body: Hormone testing is usually combined with basic blood tests and other screenings to ensure the body is ready for pregnancy, both in terms of fertility and overall health.
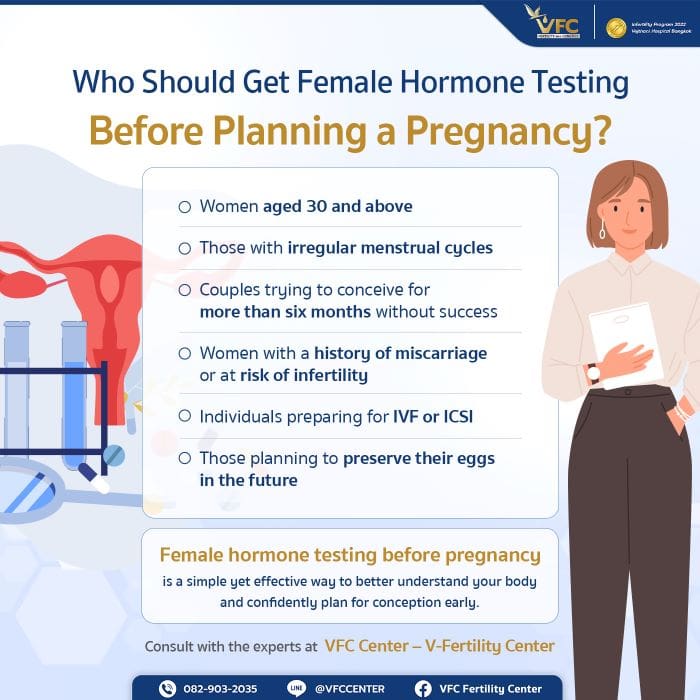
Who Should Get Female Hormone Testing Before Pregnancy?
- Women aged 30+ who have never been pregnant
- Couples trying for 6–12 months without success
- Women with irregular or absent menstrual cycles
- Women with a history of miscarriage or a family history of infertility
- Women planning IVF or ICSI
What to Do After Hormone Testing?
- Normal results: Plan pregnancy naturally or follow dietary and exercise advice.
- Abnormal results: Doctors analyze hormone results along with health and menstrual history to create a treatment plan, which may include ovulation induction, medication, or fertility procedures.
If you are planning a pregnancy and detect abnormal hormone levels, infertility screening is a crucial step to provide targeted advice and increase your chances of conception.
At VFC Center (V-Fertility Center), our experienced doctors offer comprehensive infertility screening in Bangkok using advanced technology. Services include FSH and AMH hormone testing, gynecological exams, semen analysis, and guidance on assisted reproductive techniques such as IVF or ICSI. Our medical team provides personalized recommendations to help couples achieve successful pregnancies.
Article by Dr. Worawat Siripoon
Contact or Book a Consultation:
VFC Center – V-Fertility Center
Hotline: 082-903-2035
LINE Official: @vfccenter

OBSTETRICS AND GYNAECOLOGY-REPRODUCTIVE MEDICINE





No Comments
Sorry, the comment form is closed at this time.